The Central Service/Sterile Processing & Distribution (CS/SPD) teams and suppliers to the department are constantly collaborating on the development and implementation of innovative products, services and technologies.
Here are seven innovation stories in the CS/SPD space that have generated value, including greater efficacy, accuracy, efficiency and safety, as well as cost savings and improved customer service to clinical teams.
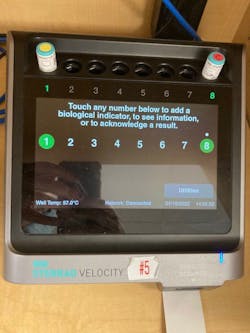
1 - Sterility validation automation increases efficiency and safety for Sanford Health
The American National Standard/Association for the Advancement of Medical Instrumentation. ANSI/AAMI ST79:2017 Comprehensive guide to steam sterilization and sterility assurance in healthcare facilities recommends a process challenge device (PCD) with the appropriate biological indicator (BI) be used at least daily, but preferably in every sterilization cycle.1
If the Joint Commission walked into your CS/SPD and asked for evidence of BI use for sterilization monitoring, how easy would it be for your team to produce accurate and complete records for their review?
When a sterile processing team manually records load monitoring, there is always the risk for human error, as Brandi Everding CRCST, CER, Manager of Sterile Processing, Sanford Health Bismarck in Bismark, N.D. explains. Her facility monitors every load with a BI – which amounts to up approximately 50 low temperature loads per day. She states:
“Just think about manually logging the BI information – lot and load numbers, BI time in/time out – for that many loads. With all the interruptions we face in sterile processing there are plenty of opportunities for error. In some cases, information would be missing from the log, which caused frustration among staff members. Let’s say you arrive for your shift and find a load sitting there with no BI time out recorded. That means extra work having to run that load again.”
Everding and her team wanted a way to eliminate manual processes to lower the risk for incomplete or inaccurate documentation and bring greater efficiency to the department.
“It’s pretty amazing because when you scan the BI into the sterilizer, the system knows to match the BI with the load and all of the data electronically transfers,” said Everding. “From a compliance standpoint, load documentation is complete and accurate. That’s what we’re looking for from a patient safety perspective and that’s what Joint Commission is going to look for when they conduct a survey. In my opinion, this system has improved this task and the workflow in our department by 100%.”
Everding’s advice to other CS/SPD teams implementing this solution: “Make sure you get everyone on board who needs to be involved – your SPD manager, IT department, a couple of super users – and work collaboratively so there is a smooth transition.”
2 - Instrument protection trays alleviate CS/SPD and OR headaches, cut down on instrument damage for Buffalo VA Medical Center
As the intricacy of surgical instrumentation continues to increase, so does the obligation of the CS/SPD and OR teams to protect these valuable assets from damage and loss. A study of one hospital’s cataract instruments repair costs found it was spending $7,361 annually – and that is for just one surgical service line.2
When Loretta Collins, Asst. Chief SPS, Buffalo VA Medical Center, Buffalo, N.Y., joined the healthcare organization, she found holes in wrapped instrument trays to be a “big issue.”
“There were a lot of headaches from the OR because they had to check for holes,” Collins explained. “Then for us in the CS/SPD, we were reprocessing trays that had already been sterilized.”
The hospital was also bearing the financial burden of repairing or replacing delicate instruments that were damaged during reprocessing or transport from the CS/SPD to the OR and back again. Buffalo’s poor water quality meant they could not use tray liners to aid in protection.
“The trays are a huge asset to our department and the OR,” said Collins. “They have an organized set-up with bumpers on them so when we do wrap them, they are less likely to get holes. This has cut down on reprocessing big time. They have also saved us money on buying new instruments because they don’t get damaged in the pan.”
When asked for her advice to other CS/SPD teams, Collins stated:
“I would tell others to do it – invest in the InstruSafe trays. When you break down how much you spend because of holes in wrap and reprocessing, the staff time and materials needed, and the cost of instrument repairs, you’ll realize that you will save money in the long run.”
3 - Instrument storage system helps UMC Tucson better meet surgery demands
Before implementing the HALYARD* and BELINTRA STERISYSTEM, Banner-University Medical Center (UMC) Tucson SPD department was struggling to effectively address the system’s influx of surgeries while simultaneously welcoming two new orthopedic surgeons who required at least 150 more tray spaces in the SPD.
“We knew we had to keep cases and scheduled procedures on track, so after hearing about HALYARD and the BELINTRA STERISYSTEM storage system, we turned to them as a new, efficient solution to the challenge at hand,” said Lester Hubbard, Senior Manager of Sterile Processing at UMC Tucson.
To ensure a seamless installation process, team members from O&M Halyard and BELINTRA started with a free, onsite assessment of UMC Tucson’s SPD – measuring the current space, understanding equipment in use and procedures, and identifying specific opportunities to maximize the space and improve workflow.
“From there, we made sure UMC Tucson had the knowledge and information needed to get the full game-changing value of the HALYARD and BELINTRA STERISYSTEM,” said Cory Ezell, North American Sales Director for BELINTRA. “All implementation work was performed by our own employees who coordinated the installation to prevent disruption to the OR and worked directly with UMC Tucson staff to ensure they felt confident in how to best use the system and maintain the new efficiencies it started to provide.”
The HALYARD and BELINTRA STERISYSTEM provided an immediate impact to UMC Tucson’s sterile processing department, according to Ezell. The facility went from processing 700 trays a week to close to 1,000 after the installation. With the STERISYSTEM, there is now additional room for 400 more trays, allowing for an increase in procedures, better ability to meet surgery demands and improved outcomes.
“With increased tray storage and decluttered space, it is now extremely easy for them to walk down an aisle and find what they need,” Ezell commented. “Before, you would see stacking and other clutter that introduced safety hazards, especially in times of staffing challenges. We know their staff has been pleased with the results and that our work has exceeded the employees’ expectations.”
“Not only did the implementation of the HALYARD and BELINTRA STERISYSTEM improve efficiencies and storage capabilities, but it also allowed us to address other problems like staffing burnout and morale,” said Hubbard. “At our facility, we have a 6,000 sq. ft. sterile processing department with 54 employees. After installation, members of the OR teams came down to the SPD to see the new layout. It was very rewarding to hear shared excitement about the new space. Though some outside of sterile processing may not realize it in the day-to-day, everything we do is aimed at improving the patient experience and providing high quality care.”
“After the STERISYSTEM installation, our employees became more excited to come to work with the storage system increasing efficiency and organization – helping them succeed and provide a high-quality patient experience,” Hubbard added. “Their feedback led to exploring and identifying innovative ways to tackle the ongoing dilemma of addressing efficiency and safety in a new way.”
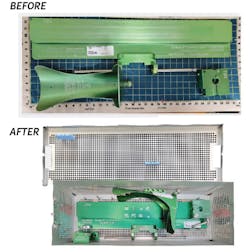
4 - Reprocessing sinks and automated flushing solutions optimize decontamination workflow and ergonomics for greater efficiency and safety
In the CS/SPD department of NorthShore Skokie Hospital, the decontamination area was generally regarded as uncomfortable and crammed, with staff members bending over sinks, manually flushing with syringes, and having low visibility due to poor lighting.
Quality of work environment changes were needed to ensure the quality of the sets coming out of the department. Additionally, enhanced ergonomics and organization would make it easier for technicians to perform at the high level required. To accomplish these goals, NorthShore Skokie Hospital implemented Pure Processing healthcare reprocessing sinks and the FlexiPump Independent Flushing System in its CS/SPD department.
Pure Processing’s sinks delivered several features that improve the quality of the working environment for technicians, including:
- Pegboards that enabled the consolidation of necessary equipment and materials to minimize movement within the department when completing tasks. Technicians also benefit from being able to see when something is out of stock or missing more readily, helping to keep necessary materials in-stock and available.
- Workflow etch plates to easily identify various areas/purposes of each sink. Coupled with the streamlined workflows realized from the use of pegboards, workflow etch plates helped make it much easier to guide new and experienced technicians through processes.
- Height-adjustability of every sink in the department allows every technician to do their work within an optimal ergonomic range, based on their height.
- Light hoods above each basin that enhance visibility.
- Timers were implemented to help technicians meet instructions for use (IFU) flush/soak requirements.
Attached to pegboard panels are FlexiPump Independent Flushing Systems, which eliminated the need to syringe flush, not only making it easier for technicians to flush devices, but reducing time spent flushing. Consistency of flushing now guarantees compliance with IFUs.
“This was our first time working with Pure Processing,” said NorthShore’s Director of Sterile Processing. “Going in, my disposition was ‘they’re just sinks.’ Now, I wouldn’t want to use anything other than Pure Processing sinks. They are high quality, but the more important aspect of this project was the customer service. We always felt supported when we had questions or needed help with something.”
Set quality has increased, processes and workflow have been optimized and clearly laid out, and the department is more well-lit, organized and ergonomically friendly throughout.
“These solutions have made it easier for staff to do the right thing, every time,” the Director added. “Team members now look forward to working in decontamination at NorthShore’s Skokie location, and technicians are generally more comfortable doing their work.
Her advice to other CS/SPD teams:
“When doing a project, it’s important to find a true partner. Pure Processing is trying to elevate technicians and the reprocessing profession. Things happen, things come up throughout a project; this truly felt like a partnership between NorthShore and Pure Processing. That’s value added beyond the products.”
5 - Containerizing loaner trays maintains sterility, saves time and money
Loaner trays present unique challenges to sterile processing. In some cases, their late arrival to the CS/SPD department means staff members don’t have enough time to properly process or review the manufacturer’s instructions for use (IFU).3
“Loaners come into facilities with only a brief time to process. The loaners we wrapped were heavy and a challenge ergonomically as there are no handles for lifting. Further, they need to be transported in multiple case carts because wrapped trays cannot be stacked. Then, if there is a puncture or tear, it now requires reprocessing. At the time ‘flashing’ was used too frequently, which is not recommended for implant trays.”
To protect the integrity of sterilized loaner trays, Mochin spearheaded an effort to move from wrapped sets to sealed containers at both Penn State Hersey Medical Center and Geisinger Community Medical Center. Her contribution was two-fold: (1) developing a justification to sterilize loaners in sealed containers and (2) listening to the customer’s voice to reduce processing times and delays with loaners.
As a result of Mochin’s efforts, both healthcare facilities made the decision to switch to SteriTite sealed containers, which are American made, compatible with all devices that can be sterilized, dry very quickly in steam sterilization, and DIN sized to accommodate DIN sized trays.
“My staff found it far easier to drop loaner trays into containers than wrap,” said Mochin. “The dimensions of the SteriTite container (width and length) were a perfect fit for the loaner trays. In some cases where the tray system was too wide for the container, we removed the wrappable outer case and lid and used the inner trays only within the SteriTite container or placed some items in an instrument basket for proper fit.”
Mochin and her team established a “lending library or loaner bank” on the clean side of their department to store the SteriTite containers for when loaner trays arrive.
The results: A happy staff and well-functioning department, greater process efficiency and better service to the customer – the OR team.
“With no more tears or punctures, the staff was very happy that sets were now in use and not returned for reprocessing,” said Mochin. “OR delays were no longer caused by reprocessing delays. We were able to reduce sterilization times, because the containerized sets were now dry in less than 10 minutes. We eliminated ‘flashing’ or IUSS so we could provide the same level of care to all patients.”
Her advice to other CS/SPD teams:
“My advice is to transition to sealed containers. Demonstrate how sterilization containers can save time and money over wrapped items. This will reduce stress, turnaround time, increase surgeon satisfaction, and contribute to the bottom line. While loaners are not hospital property, placing them in containers may in the end show the greatest savings to the facility, as one container can be used frequently for any set coming in and out of the facility. More turns, more value.”
6 - Automating robotic surgical instrument reprocessing drives efficiency and consistency
In 2018, the U.S. Food and Drug Administration (FDA) provided guidance around reprocessing instructions for reusable medical devices, which includes robotic surgical instruments. This FDA guidance outlined requirements for manufacturers of washer/disinfectors to validate reprocessing instructions, specifically when indicating them for use with reusable medical devices, such as with da Vinci EndoWrist instruments.
“The only reprocessing option was to process da Vinci EndoWrist Instruments using a labor and time intensive manual process,” said Sarah Brown, Senior Product Manager, STERIS. “Customers sought out Intuitive and STERIS asking for a solution that automated the cleaning process for these complex devices. STERIS and Intuitive worked together to help simplify the automated cleaning process, creating easy-to-follow instructions that help create cleaning outcomes consistent with the manual cleaning process.”
They added a RAS (Robotic Assisted Surgery) cycle and racks to the AMSCO 7000HP washer/disinfectors to help facilities reduce the soak time and completely eliminate ultrasonic cleaning for select devices. The process reduces the number of manual steps at the sink for cleaning select da Vinci EndoWrist devices by using the 7000HP washer/disinfectors and RAS cycle and Racks to clean da Vinci EndoWrist devices.
“We have seen many customers adopt the use of the RAS Racks and Cycle and transform their process for cleaning da Vinci EndoWrist instruments,” said Brown. “They are able to reduce total processing time without sacrificing consistent cleaning outcomes.”
One customer using the AMSCO 7000HP washer/disinfectors with RAS racks and cycle is Memorial Hospital, Jasper, Ind. Toni Cibak, CST, CRCST, the hospital’s Sterile Processing Manager comments on the benefits:
“Our STERIS 7053HP Washer/Disinfector with RAS cycle has been a game changer. The RAS cycle that washes da Vinci [EndoWrist] instruments saves us time. Previously, we had to wash them in our ultrasonic and then washer to clean them. Now we have a special rack and cycle to do the same thing. It saves us steps and time.”
7 - Off-site sterile processing serves multiple hospitals with increased accuracy and efficiency
Space is often at a premium for healthcare facilities based in urban areas. With surgical volumes growing along with the number of instruments and devices that must be reprocessed, it can be a tight squeeze to include a large enough CS/SPD department to meet a hospital’s needs.
A major metropolitan hospital system on the East Coast was in the process of designing a new hospital in the city center, but without a sterile processing department onsite. They had a desire to create a central processing area offsite that would manage five hospitals across the network, so space was needed to consolidate these separate entities to one single location. This “surgical warehouse” is intended to house not only all surgical instrument trays, but also soft goods as well.
The hospital system implemented a “just-in-time” (JIT) distribution philosophy and new trucking distribution model that delivers case carts into each individual hospital only as needed. They deliver carts from the offsite CS/SPD the day before scheduled surgeries, and later retrieve used materials for reprocessing offsite.
As Craig Sinclair, Manager of Systems Integration & IT with Hänel Storage Systems, explains, JIT is meant to increase efficiency and decrease waste by receiving supplies only when needed for surgeries, which in turn reduces inventory costs inventory and increases inventory turnover.
“All materials are sterilized and packaged outside the hospital environment, which was a completely new process,” said Sinclair. “Also new was the majority of picking labor. Rather than use sterile processing specialists at a satellite location separate from the hospital, the SPD model was turned into more of a distribution center model.”
The offsite CS/SPD employs warehouse and distribution center specialists who are experienced in picking and placing inventory items from a pick list. “In this way, the surgical instruments and soft goods are just a different type of item found in a warehouse,” Sinclair explains. “Think of an Amazon distribution center on a smaller scale, but with only SPD inventory.”
According to Sinclair, the results have been unique in the industry: An offsite CS/SPD that serves multiple hospitals at the same time, while increasing accuracy and efficiency at each respective location.
“Don’t discount creating a new strategy culled from best practices found in a different industry,” Sinclair added. “There are tried and true business models from other types of businesses that can be applied to in a hospital environment if you’re open to changing your paradigm.”
8 - Automated sterility expiration date tracking drives compliance for a growing number of health systems
In its Guideline for Disinfection and Sterilization in Healthcare Facilities (2008), the Centers for Disease Control and Prevention (CDC) states: “Any item that has been sterilized should not be used after the expiration date has been exceeded or if the sterilized package is wet, torn, or punctured.”4
Peter Hawryluk, Account Executive, MedVantage, notes how this presents a what comes first, “chicken versus egg” scenario for CS/SPD teams. He states:
“Hospitals used to do things based on the integrity of a sterile package. A tray was always assumed sterile unless it was damaged, open or wet. Now hospitals are noticing that instrument manufacturers want them to manage integrity by sterilization expiration date. So, what comes first - the expiration date or integrity of the package?”
Hawryluk says he sees a growing number of hospitals switching from event related (e.g., hole in wrap) to time related (e.g., expiration date) sterility monitoring. For these facilities the challenge lies in keeping track of when trays have been sterilized and when they are set to expire.
“Our SteriDate system captures expiration dates for facilities and fulfills that need,” said Hawryluk. “It automatically captures the date a tray has been sterilized and includes the corresponding fixed expiration date. The user can print a label from the system to affix to the tray that includes the expiration date, sterilizer number, cycle/load number and the initials of the employee who ran the load.”
Hawryluk says customers can choose from a variety of label formats, including those color coded by sterilization expiry (e.g., yellow for 180 days, red for 265 days, etc.), to serve as a visual aid in helping the CS/SPD team manage trays in sterile storage. The system alerts users to trays nearing expiration. The system also allows users to record event-related sterility breaches, such as when a tray’s wrapping is found damaged, open or wet.
“We find that once a flagship hospital in a system adopts the technology, the rest of the hospitals in the system soon follow,” said Hawryluk. “It’s a great way to standardize.”
References:
1. Importance of Following Standards and Guidelines, ASP, https://www.asp.com/en-us/education/articles-and-white-papers/aami-standards
2. Eye Tray Study, Instrusafe, Summit Medical, https://www.instrusafe.com/cost-savings/
3. A Better Package for Loaners, Case Medical, July 6, 2022, https://casemed.com/index.php/resources/blog/item/116-managing-your-loaner-and-consignment-process
4. Guideline for Disinfection and Sterilization in Healthcare Facilities (2008), the Centers for Disease Control and Prevention (CDC), https://www.cdc.gov/infectioncontrol/guidelines/disinfection/sterilization/sterilizing-practices.html

Kara Nadeau | Senior Contributing Editor
Kara Nadeau is Sterile Processing Editor for Healthcare Purchasing News.