Central sterile/sterile processing department (CS/SPD) professionals have access to a number of industry standards and guidelines that offer recommendations and best practices for the effective and safe processing of instruments from organizations such as the American National Standards Institute (ANSI), Association for the Advancement of Medical Instrumentation (AAMI), Association of periOperative Registered Nurses (AORN) and ASTM International.
In addition, the manufacturers of surgical instruments and devices provide instructions for use (IFU) for each of their products, which offer step-by-step requirements for processing from decontamination through sterilization (and beyond).
Furthermore, manufacturers in the sterile processing space offer numerous products designed to help CS/SPD professionals test and monitor the effectiveness of their equipment and processes, including physical monitors, internal and external chemical indicators and biological indicators.
With all of these resources at their fingertips, why is it so difficult for the CS/SPD to ensure the sterility and quality of the instruments and devices they are processing?
In this article we explore some of the challenges faced by CS/SPDs as they work to deliver safe and effective instruments for patient care; recommendations from CS/SPD professionals, industry associations and manufacturers on how to ensure the quality and sterility of instruments despite these challenges; and new products that CS/SPDs can use to help stay compliant and keep patients safe.
Why is it so hard?
The obvious challenges to CS/SPD quality assurance include the increasing complexity of surgical instrument technologies, changing and evolving standards/regulatory requirements and the time and effort required to process them, and pressures from the operating room (OR) and other customers to quickly turn around instrument sets. Underlying these issues are inadequate staffing levels, insufficient education, and IFUs that are unclear, overly complex, and in many cases contradictory to one another.
“Many CS/SPD professionals repeatedly hear ‘quality over quantity,’ but then face the anguish of the circulator or surgeon who asks why instrument sets were not completed,” said Natoria Pettyjohn, CSPDT CSIS, CFER who is a Technician II representative to the Certification Board for Sterile Processing and Distribution (CBSPD). “Poor staffing, insufficient training, and education are some of the many challenges SPD professionals face today.”
Insufficient staffing
A major problem that many CS/SPDs face is their hospitals staffing their departments based on productivity measures that do not take into account the time and effort required to produce a quality product for the operating room (OR) or other customer, explains Damien S. Berg, BA, BS, CRCST, President of the International Association of Healthcare Central Service Materiel Management (IAHCSMM) and SPD Manager for St. Anthony Hospital, in Lakewood, CO.
“No matter what we write in the standards we will not impact quality in sterile processing until we rethink our staffing model, particularly in decontamination where issues can impact workflow all of the way down the line,” said Berg.
The underlying issue of IFUs
Compounding the issue of insufficient staffing levels are the IFUs themselves. Today there is no standard IFU format; therefore, manufacturers of similar instruments have IFUs that not only look different, but also have very different contents and requirements for the effective processing of their devices.
While most CS/SPD professionals will say they follow each and every IFU to the letter, its common knowledge within the industry that deviation does occur in the face of productivity demands, with departments coming up with processing methods that leverage commonalities across instruments. In some cases they have no choice but to use their individual knowledge and expertise in an attempt to reconcile all of the IFU variables.
IAHCSMM President-Elect Tony Thurmond, CRCST, CIS, CHL, Manager of Central Services, The Christ Hospital in Cincinnati, points out that in other cases, the IFUs are not specific enough, lacking the detail necessary for CS/SPD professionals to adequately process the instruments.
“Most manufacturers have a generic IFU for all of their instruments, which does not always identify the focus that a sterile processing professional needs,” said Thurmond. “For example, the cleaning process for a Frazier suction tip is different that a curved hemostat, yet, often the IFU is the same.”
The AAMI Workgroup 12 has been tasked with developing standardized cleaning protocols for specific categories or “families” of instruments to make it easier for CS/SPDs to follow, and increase adherence to the manufacturer’s recommendations (see the March 2018 HPN article: The pitfalls and triumphs of IFUs). Berg is Co-Chair of the workgroup along with Ralph J. Basile, Vice President of Healthmark Industries.
“I believe standardized instructions for use will allow staff to identify and read more clearly the process and how to clean, inspect and prep the instrument for sterilization,” added Thurmond.
Doing without knowing
The CS/SPD has access to a wide array of equipment to decontaminate, clean and sterilize instruments, as well as an assortment of physical, biological and chemical indicators with which to verify cleaning and sterilization success. But as Berg points out, the value of these tests are dependent upon the knowledge of the individual using them.
“The big gap I see between decontamination and sterilization is the quality assurance on testing — the why, when, what and how we test for cleanliness, including verification that the manual processes or mechanical washers work,” said Berg. “Because there are certain things these tests tell you, and certain things they don’t tell you. You could be testing inappropriately and get false results that steer you down the wrong path.”
Berg believes the industry needs solid guidelines on testing and monitoring in the CS/SPD, clearly stating this is when one should test, this is what they should test and this is how they should test in various scenarios.
Assuring quality: Steps you can take today
While industry’s efforts to address staffing levels, IFU standardization and quality assurance testing/monitoring guidelines are longer-term goals, there are steps CS/SPD professionals can take today to improve quality in their departments. The following are tips, best practices, products and programs designed to help CS/SPDs in their quest for quality and sterility assurance.
Get it clean
“An instrument can be clean without being sterile, but it can’t be sterile without being clean,” said Noreen Costelloe, Director of Marketing, Ruhof Healthcare. “This statement supports the well-known fact that cleaning — the removal of organic and inorganic debris from an instrument or device — should precede all disinfection and sterilization processes. Failure to do so can interfere with microbial inactivation and can compromise the disinfection or sterilization process, placing patients at serious risk. Therefore, one key area that CS/SPD professionals must address as part of their quality assurance plan for sterilization is the monitoring of/and verification that instruments and devices have been properly cleaned.”
The Ruhof ATP Complete Contamination Monitoring System is a rapid, simple and reliable method for verifying the effectiveness of the cleaning and decontamination process for the outer surfaces and internal channels of scopes/cannulated instruments and surgical instruments, along with all noncritical facility surfaces. The system detects adenosine triphosphate (ATP), the universal energy molecule found in all animal, plant, bacterial, yeast and mold cells. Product residues, particularly blood and bioburden, contain large amounts of ATP while microbial contamination contains smaller amounts of the molecule. The Ruhof ATP Complete measures the amount of contaminants present after cleaning.
“Operational qualification and regular performance qualification are the only ways to ensure cleaning processes are effective in reducing the risk of passing infections through surgical instruments,” said Pawel de Sternberg Stojalowski, Founder and Managing Director, Aseptium. “What gets measured, can be verified and monitored, and process challenge devices are a simple and effective tool for ensuring the quality of reprocessing.”
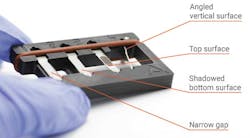
Aseptium’s family of VeriTest Process Challenge Devices (PCDs) assesses and monitors the cleaning effectiveness of surgical instruments. The PCDs are based on natural protein test soil that contains animal blood and tissue representing realistic contamination found on surgical instruments. CS/SPD professionals can use the devices to test the cleanliness of difficult to clean instruments, containing such elements like narrow gaps found in scissors and clamps, shadowed areas where instruments or their parts block the fluid from reaching all contaminated surfaces, as well as horizontal and vertical surfaces. The company refers to it as “four dimensional cleaning evaluation.”
Set your sterilizer’s baseline
“A key area that is neglected is proper qualification of equipment upon installation,” said Jonathan Wilder, Ph.D., Managing Director, Quality Processing Resource Group. “AAMI ST79:2017 mentions installation qualification (IQ), operational qualification (OQ) and performance qualification (PQ) after installation. These provide you with a formal set of baseline measurements for sterilizer performance for your unique combination of location, workplace environment and utilities. This process shows you, in detail, what the sterilizer can and will do when it is new, and, in a proper set of testing, also helps to iron out any utilities issues, like wet steam and deficient vacuum. This is required in other countries, like the UK and Germany, and is part of the basis for their not needing to use as many indicators as we do in the US. Should we do any less?”
Quality Processing Resource Group offers a Sterile Processing Total Support Service, which is an independent check of a CS/SPD’s conformity to best practices as defined by AAMI, the Joint Commission and the Centers for Medicare & Medicaid Services (CMS). In addition, the service provides a deep technical dive into the function of a department’s washers and sterilizers, and provides adjustments and recommendations for system modifications to get machines to optimal function.
Apply the standards and invest in education
“A successful sterilization quality assurance program requires the facility to obtain the knowledge, decipher the sterilization quality assurance guidelines outlined in ANSI/AAMI ST79 and implement a robust sterilization quality assurance program into a routine well-documented process,” said Amanda H. Coss, CSPDS, CSPM, CRCST, CIS, CHL, National Education Coordinator, Mobile Instrument Service & Repair.
But simply sharing the standards isn’t enough. As Coss points out, CS/SPDs must provide hands-on training and education to their staff members on how to apply the standards to their work at hand in order to have a real impact on quality.
“The education behind this process provides a firm understanding of the how and why these processes are carried out,” said Coss. “When people are empowered with education, they are not only likely to understand the importance of the process, but can help improve upon the quality process itself.”
“The ANSI/AAMI ST79: 2017: Comprehensive guide to steam sterilization and sterility assurance includes a number of revisions impacting sterile processing workflow. As these standards continue to evolve, CS/SPDs must evolve with them,” explains Lena Burgess, CRCST, CIS, CFER, CHL, Senior Manager, Clinical Services, Compliance and Safety, STERIS Instrument Management Services.
“The ongoing education required to keep SPD personnel up-to-date on the latest industry standards is of utmost importance in a quality assurance program,” said Burgess. “With industry experts endlessly working to improve patient safety and surgical outcomes, there is a huge need for continuous education for SPD personnel development.”
Key Surgical offers an education program that focuses on important topics in the sterile processing industry, including quality assurance. It is a set of virtual learning labs designed to be simple, fun and interactive. Each course includes an interactive quiz based on the information learned, and upon completion users earn continuing education credits (CEs), accredited through IAHCSMM and CBSPD.
“Ensuring that sterile processing staff have a foundation of industry knowledge and access to continuing education resources is the cornerstone of a successful quality assurance program and effective sterile processing department,” said Brandon VanHee, Clinical Education Manager, Key Surgical.
Teach the why, when and how of testing and monitoring
“Load monitoring is very important,” said Paul Girouard, Senior Category Manager, McKesson Medical-Surgical. “To have complete load monitoring we must have the mechanical, chemical and biological monitors in place. All of these monitors are equally important and loads should not be cleared without verifying all of these aspects. Policies and education help inform and prepare staff to ensure they are completing the load monitoring effectively. Healthcare facilities should have such policies and education in place for sterilization and high level disinfection.”
Although the industry has a long way to go when it comes to the development of standard quality assurance testing and monitoring guidelines, Berg urges individual CS/SPDs to start today by helping their staff understand why these tests are needed, when they are needed, how they work and what results they can and cannot provide.
“That’s where education and understanding comes in — a CS/SPD professional needs to know he/she is running this biological because of X, Y and Z, or using this chemical indicator for this reason, comprehend the results and then act on them appropriately.”
Steve Kubler, U.S. Marketing Manager in 3M‘s Device Reprocessing division, suggests setting up simple, standardized protocols for load monitoring as a way to support quality assurance in the CS/SPD. He states:
“Having a standardized workflow process can help ease staff training and provide consistency of action to help reduce factors for error. For example, a facility could set up a standard protocol to monitor every load with a BI across all sterilization modalities used. Setting up this practice could help reduce the complexity of execution while elevating the standard of care. Of course, every department leader will need to conduct a cost-benefit analysis to see what makes sense for them and the types of facilities they oversee.”
The 3M Attest Dual Auto-reader technology helps facilities simplify, standardize and streamline sterilization processes by incubating and providing results for both Attest steam and vaporized hydrogen peroxide (VH2O2) biological indicators (BIs). The Attest Dual Auto-reader provides quick, accurate BI results in 24-minutes so SPDs can verify that every load has met sterilization parameters before being released to the OR.
Define expectations
“To sustain a compliant culture, staff and leadership must have defined expectations. Defined expectations are established through detailed standard work instructions that outline steps in a process,” says Deana Ward, BSN, RN, Sr. Consultant-Professional Services, STERIS. “Competencies and staff education tools are then derived from the written standard work instructions and should incorporate the physical, biological and mechanical monitoring steps. These defined steps and tools are then used by shift and department leadership to monitor accountability through observations and measurable indicators which trend process and quality compliance.”
To assist CS/SPDs in this effort, STERIS IMS Professional Services offers consultants who partner with customers to perform clinical, operations, capacity, strategy and staffing assessments to assist in the development of processes and quality improvement initiatives.
Check for competency
“Sterile processing professionals can improve their quality assurance by improving and constantly updating their competency checklists,” said Thurmond. “I feel that competencies are sometimes used once a year to sign off a technician. But what happens during the rest of the year – does the technician go back to old habits? By doing a walk through the department, identify someone who may have had a challenge with a tray or process, and review their competency with them. Also, a lot of competencies may ask for verbal explanation, but a full demonstration is the preferred method of verification.”
Continuously challenge quality systems
“The complexity of new surgical equipment continues to increase, and so does the cleaning and processing of that equipment,” said Pika Lynch, RN, MSN, Director, Clinical Services, TSO3. “Work towards preventing errors before they occur and utilize processing technological advances to your advantage, including ATP testing, routine culturing programs, borescope examination, sterilization in lieu of HLD and standardized, documented quality check systems at multiple stations within sterile processing. Communicate your findings with staff and encourage open transparent communications within the department to ‘stop and report.’ Make the emphasis on near misses and not misses because if contaminated instruments make their way to a patient, it is already too late. If a near miss occurs, be sure to evaluate the actual process and not just the person processing the equipment.”
The TSO3 STERIZONE VP4 low temperature sterilizer offers the lowest cost per instrument sterilized (versus other low temperature H2O2 systems), and significantly increased throughput with up to 75 lbs of mixed, general instruments.* It features just one cycle – starting at the push of a button. The STERIZONE VP4 is the only sterilization system validated and FDA cleared to terminally sterilize long, flexible endoscopes, such as duodenoscopes, colonoscopes and gastroscopes.* It can sterilize three sets of robotic surgical tools simultaneously, and sterilize batteries at the same time as orthopedic tools.
* See claims at www.TSO3.com
Think outside of the CS/SPD
Logically, the more a product is handled, the more likely it is that that product can become contaminated,” said Nancy Pakieser, Senior Director, Industry Development, TECSYS. “Manual replenishment, searching for recalled product, cycle counting and other non-automated processes each call on staff to physically touch product, at each instance increasing the risk for contamination, not to mention are disruptions to clinical activity. Technologies that allow for visibility of the supply chain allow organizations to make improvements to operations that can control those touch points and cut down on that risk.”
Continuously improve
“When developing an SPD quality assurance program, the SPD professionals should focus on process improvement, along with implementing attainable goals,” said Pettyjohn. “As change happens, they should update policies and procedures to coincide with the standard of work. Ensure that it’s not just the soup of the day. SPD professionals need to be consistent in reviewing metrics that will provide data with the department’s successes and barriers.”

Kara Nadeau | Senior Contributing Editor
Kara Nadeau is Sterile Processing Editor for Healthcare Purchasing News.