Stroll into any surgical facility that operates a case cart system and it’s likely that you will find case carts strewn about the surgical floor, the sterile processing department, and every hallway in between. Even in the most well run perioperative systems case carts present a unique set of challenges; from storage and staging, to case picking, to transport, to system ownership. How can something so simple at first glance be so difficult in practice?
Too often such difficulties arise from inadequate and/or ineffective planning during the design, procurement, and implementation process. However, these headaches are avoidable. Investing time and effort in a thorough, well executed, systems approach to planning and design pays dividends in the future. Through application of industrial engineering (IE) concepts such as Lean methods, discrete event simulation, and operations research, just to name a few, a case cart system can be designed and optimized in such a way that allows for efficient, effective, and responsive operation. Such an operation directly enables the delivery of cost effective, high quality, patient-centered surgical care — the goal of all health care organizations.
Engineer the approach
Peter Senge, an American systems scientist who wrote the influential book The Fifth Discipline, defines systems thinking as, “…a way of thinking about, and a language for describing, the forces and interrelationships that shape the behavior of systems.”1 Systems thinking is extremely effective when solving complex, interrelated, multi-layer problems such as planning, implementing, and managing a case cart system. Systems thinkers not only examine system components, but also examine the interactions and relationships between these components; a step that is all too often omitted during the planning process. Obviously, before applying such an approach the system in question must be defined. Two IE tools — the value stream map and process flow chart — are particularly well-suited for this task.
A value stream map (VSM) is a Lean method for analyzing the flow and state of materials, resources, information, and related data through a system. A well-constructed VSM starts and ends with the customer. A process flow chart complements the VSM by defining the sequence of inputs, outputs, actions and decisions within a system. When creating a VSM and process flow chart for a case cart system consider the following:
- Who is my customer? Is it the patient? Is it the clinical staff?
- What materials flow through my system? (case carts, instrument kits, supplies, etc.)
- What resources flow through my system? (nurses, surgeons, patients, staff, etc.)
- What type of information flows through my system? (patient records, preference cards, verbal communication, etc.)
- Does the state of materials, resources and/or information transform within the system? (clean/soiled, available/occupied, etc.)
- What actions must be taken to prepare a case cart for a procedure? What decisions must be made during this process?
After creating a VSM and process flow chart, revisit each and apply systems thinking; identify and document the interactions and relationships within the system. How does one element within the system effect another? Doing so will ensure a comprehensive understanding of intended operations, identify system features that require in-depth analysis, and detect potential points of failure.
“Right Size” the fleet
Constructing a VSM and process flow chart in the early stages of planning is extremely worthwhile for all involved. These documents can be used by the design team to solicit feedback from stakeholders and generate valuable dialog. They can be used by equipment planners and procurement specialists to identify the quantity and duty of equipment required to enable case cart operations. They can even be used by OR managers and administrators to implement and manage their new case cart system. As an added benefit, a well-constructed VSM and process flow chart can be used to determine the optimal size, or “right size”, a facilities case cart fleet. Not only does this ensure that the proper number of case carts are purchased, but also ensures that adequate staging and storage space is captured for carts within the sterile processing department and on the surgical floor.
A number of mathematical approaches — some simple, some complex — can be used to estimate the number of case carts required to serve a surgical platform. Simple calculations based on cases per day and carts per case can be used to quickly “bracket” the size of a case cart fleet. For instance, maximum fleet size can be estimated by assuming that every case will require its own case cart (i.e., no turn over; a case cart cannot be used more than once per day). In other words, the maximum fleet size is equal to the average number of daily cases. While useful in some instances, these estimates do not mirror reality. Surgical systems are notoriously complex; they have many components and are inherently variable. While the accuracy of simple calculations can be improved by considering additional information to include the number of carts per case (i.e., case complexity) and turn-around time (i.e., processing speed) they are far too simple to capture the interactions and relationships between the processes, resources, and information involved in a case cart system. Luckily, discrete event simulation is a perfectly suited mathematical tool.
Simulation and modeling
Discrete event simulation (DES) is a powerful tool used by engineers to define a complex process as an ordered set of distinct, well-defined events, much like those in a process flow chart. DES enables an engineer to quickly and efficiently study complex interactions and relationships between system components and account for variability while measuring their effect on system performance. (See Figure 1.)
Just like the systems they evaluate, every DES model is unique. No two institutions operate in the same manner, and therefore require a tailored solution. Despite this fact, the basic steps involved in DES modeling remain constant:
- Define the system as a series of distinct events (i.e., processes, decisions, etc.).
- Create statistical distributions that describe each event (i.e., length of case, type of case, processing time, etc.).
- Constrain the system with resources and schedules (i.e., people and/or machines).
- Run the model multiple times (referred to as replications) and collect model outputs.
- Analyze outputs, adjust the model, and test alternatives as appropriate.
Outputs from such a model are often the subject of statistical analysis and used to generate key performance indicators (KPIs) that describe system performance. In turn, these KPIs can be used by the design team, project stakeholders, and facility leadership to make thoughtful, well-informed design, procurement, implementation, and management decisions. Furthermore, simulation allows one to experiment with design alternatives with little to no additional cost.
Case study: Case cart simulation in action
Calculating the number of case carts required to serve a surgical platform is crucial to making well-informed procurement and design decisions in a new facility. At one such facility, located in eastern Massachusetts, a simulation strategy was applied to right-size the cart fleet and ensure adequate staging and storage space for the fleet within the facility.
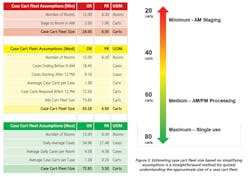
To begin, simple estimates were established by calculating maximum, medium, and minimum fleet size based on historical case history. Assumptions were made to simplify the calculations and quickly arrive at defined range.
- Maximum (conservative) — a case cart can be used only once per day.
- Medium — a case cart returned to the SPD before 9AM can be used again after 12PM.
- Minimum (aggressive) — a case cart used for a case before 12PM can be used again after 12PM.
Using the assumptions above, it was estimated anywhere between 24 and 76 case carts would be required to serve the twelve (12) OR’s planned for the facility. It was likely that the actual value would be near 64 carts, as determined by the assumptions used in the medium scheme. (See Figure 2.)
After calculating an estimated fleet size, a DES model was constructed to further refine the fleets intended size. First, statistical distributions to describe surgical schedule, length of procedure, and case carts per case were constructed from historical data obtained from the institution. Such distributions are used by the model to generate demand all while accounting for variability and reflecting the unique needs of the facility. Next, a processing workflow was defined. This workflow accounted for the various steps involved in preparing a case cart (i.e., transport, stripping, washing, drying, picking, etc.), as well as the resources required to do so (i.e., sterile processing technicians, cart washer/disinfectors, etc.). Finally, the model was configured and verified against current state data and user expectations.
Outputs of the model were used to define the number of case carts required to serve the ORs planned for the facility, as well as the maximum number of carts that would could be expected to reside at any location in the facility, such as soiled utility rooms, the sterile processing department, or the sterile core. Upon completion, the simulation model indicated that approximately 56 case carts, plus or minus 5, would be required to serve the OR system. As expected, this value fit within the range determined by estimation, and was near to the medium scheme value. Statistical robustness added by the simulation model made it highly likely that the actual number of case carts required in the future would be near this value. In turn, these quantities were used by the projects equipment planners to budget for and procure case carts and by the design team to appropriately size the sterile core, sterile processing department, and soiled holding rooms.
Implement best practices
Even after creating a VSM, process flow chart, and discrete event simulation model there are still many industrial engineering concepts that can be applied to avoid headaches in the future. These concepts take the form of best practices, many of which find their roots within manufacturing and distribution systems — the traditional focus of industrial engineers. These concepts include:
- Slotting — Slotting is an industrial practice whereby fast moving items are placed in locations that are easy to access and restock. Slow moving items are placed in less accessible locations that may require a staff member to travel a greater distance to acquire. A well slotted SPD will dramatically increase the overall performance of a case cart system.
- Just-In-Time (JIT) Processing — JIT processing is a strategy developed and perfected by Toyota whereby efficiency is increased and cost decreased by receiving goods only when they are needed. A JIT case cart operation delivers instrumentation, surgical supplies, and case carts to the OR when needed, in the quantity needed, in the state needed. Implementing a JIT philosophy when implementing and managing a case cart system ensures that neither the surgical floor nor sterile processing department is overwhelmed by clean or soiled case carts.
- Eliminate Waste — in any system, it is crucial to eliminate wasteful, non-value added activities to include excess travel, double handling, waiting, underutilized resources, and rework to name a few. Eliminating waste (sometimes referred to as “muda”, the Japanese word for waste) increases efficiency while decreasing cost.
By no means are these the only principles that should be considered when planning a case cart system, however, it’s likely that application of these three concepts will dramatically reduce the likelihood of implementation and management difficulties in the future.
Though a relatively new trend, engineers have adapted their skill set to the health care industry and have remained focused on increasing efficiency, quality, and patient safety while decreasing cost and errors. In a day and age when health care organizations are continually asked to do more with less in an ever increasingly complex environment, the role of a systems thinker is an important one.
Derrick Bransby is a project engineer at St.Onge Company (www.stonge.com) York, Pennsylvania. He specializes in applied industrial engineering within health care systems. His focus rests on designing support systems and supply chains in health care facilities with an eye toward efficiency and quality. He has worked with Johns Hopkins Medicine, Duke University Medical Center, and Boston Children’s Hospital. Derrick received his BS in industrial engineering from the University of Pittsburgh and is a MBA candidate at the Johns Hopkins University Carey Business School.
1. Senge, P. M. (1994). The fifth discipline fieldbook: Strategies and tools for building a learning organization. New York: Doubleday/Currency.