A healthy patient who was expected to make a full recovery from a routine surgical procedure is found dead in bed from an unintentional opiod overdose. Another patient developed severe internal hemorrhaging and a near-fatal infection caused by a surgical sponge that was mistakenly left inside the patient’s abdominal cavity. These and other disturbing medical mistakes are also referred to as Never Events — and for an obvious reason — they should never happen. Not only are Never Events harmful to patient-victims, but healthcare givers can also suffer emotional and psychological distress. Medical errors such as these are also bad news for a medical facility’s budget and reputation.
According to the Agency for Healthcare Research and Quality, the National Quality’s Forum list of Never Events consists of 29 events grouped into 6 categories: surgical, product or device, patient protection, care management, environmental, radiologic, and criminal.1 Among the most common Never Events are unintended retention of a foreign body; wrong-patient, wrong-site, wrong-procedure; fall; operative/postoperative complication; and medication error.
The Joint Commission’s Sentinel Events include Never Events. Anne Marie Benedicto, MPP, MPH, Vice President, The Joint Commission Center for Transforming Healthcare, commented on the magnitude of medical error. “A 1999 report by the Institute of Medicine estimated that up to 98,000 people a year die [in the US] because of mistakes in hospitals; subsequent reports have said the number is much higher.”
Anne Snowdon, RN, BScN, MSc, PhD, Chair, Odette School of Business, University of Windsor, Ontario, Canada, voiced the concern of many that the number of Never Events may be vastly underreported and the true number unknown. “Medical error is now the third leading cause of death in North America, third only to heart disease and cancer. Adverse events—medical error and Never Events—are reported on a voluntary basis. Thus, we have limited data that quantifies how often Never Events occur.”
Fixing a flawed system
Occurrence of Never Events may indicate a fundamental problem in a healthcare facility: a lack of a culture of safety.1 “There is growing understanding that most errors that contribute to harm are the result of flawed systems and processes, not the rogue or negligent actions of individuals,” stated Benedicto.
Benedicto believes an integrated approach to patient safety creates a high level of safe patient care that can safeguard against Never Events. “The past decade has brought increased focus on high-reliability organizations (HROs). HROs perform at consistently high levels of quality and safety despite the potential for large-scale harm. This is a level of performance that has not yet been met by a single healthcare organization. To assist healthcare organizations on their high-reliability journey, The Joint Commission created a framework for high reliability that is specific to health care. The High-Reliability Health Care Maturity Model has three foundational domains: leadership commitment to zero harm; a fully functional safety culture where employees speak up to identify unsafe conditions; and employees address opportunities for improvement because they are skilled in robust process-improvement tools such as Lean Six Sigma and change management.”
Reporting of unsafe conditions involves trust. Creating an atmosphere of trust has been a challenge in healthcare facilities. Many healthcare workers fear repercussions from reporting less-than-stellar conditions or adverse events.
Martin A. Makary, MD, MPH, FACS, Professor of Surgery, Johns Hopkins School of Medicine, and author of the New York Times Bestseller “Unaccountable,” believes, “Transparency is a terrific concept in principle, but it has to be done with the goal of improvement rather than the goal of shame. Moreover, transparency efforts should ensure a level playing field for comparing centers, use understandable language and metrics, and be sure not to punish doctors and hospitals caring for populations that may have higher risk factors for the outcome being made transparent.”
Benedicto, The Joint Commission, believes that diligent reporting of all patient-safety events can lead to a learning environment within the hospital that fosters trust and encourages reporting. “Trust is the foundation of a safety culture, leading concerned employees to report unsafe events and identify opportunities for improvement,” asserted Benedicto. “When leadership responds positively to these opportunities, employees are then further motivated to report, which results in more improvement and builds greater levels of trust. It is vitally important that the reporting system is linked to an organization-wide structure and methodology for addressing improvement opportunities. Trust will flourish when employees see their reports acted upon, and the results of the improvements will keep patients safer while transforming an organization.”
Snowdon, University of Windsor, talked about other challenges encountered in establishing a culture of safety and linked success toward that goal to the supply chain. She pointed out that the food-supply system is better equipped to trace product than is the healthcare system. That should be unacceptable. “The most significant challenge is the complete lack of tracking and traceability of products, care procedures, and patient outcomes in global health systems. We can track and trace a food item from the farm to the consumer who purchased the item, bar coded by lot and batch number for full traceability. In health systems today, we have no ability to track what products—devices, medications, etc.—are used or implanted into which patients, when, where, and by which provider teams. There is no system infrastructure in clinical settings to provide the tracking and traceability of medications or products used so that clinicians would have a double-check and alert system to prevent errors from occurring proactively.
“In our recent study, we proposed how Never Events could be almost completely eradicated, simply by placing bar-code scanning infrastructure into clinical environments,”2 said Snowdon. “If supply chain infrastructure were implemented in health systems, clinicians would have the tools to scan the bar code of every product to every patient identification band and to every provider identification to offer a digital and automated double check that the right procedure and right products are used for each and every patient in healthcare systems.”
Snowdon cited the experience of a hospital in Ontario that has documented an astounding 90 percent decline in medication-related Never Events within one year of implementing this bar-coding infrastructure. Their goal is to achieve 100 percent eradication of Never Events related to medications hospital-wide in this particular organization.
Makary concurs that technology is one good solution for preventing Never Events. He talked specifically about the number 1 Never Event, retention of a foreign object following surgery.
“With modest or heavy surgical volumes, most hospitals report having a few retained foreign objects inadvertently left during surgery each year,” said Makary. “In addition to the potential human tragedy, it’s a problem that deeply frustrates docs, nurses, risk managers, and hospital leaders alike. One reason we don’t hear as much about them as we might is that (1) non-disclosures are routinely a part of any hospital settlement with a patient or their family, and (2) they are embarrassing to talk about. But, they remain the Achilles heel of a surgical tour-de-force of surgical technique and sophistication.”
In considering the effect of current efforts to impose accountability, such as nonreimbursement and public reporting, Makary observed, “While some of these efforts have yielded some improvement, what really moves the needle is re-designing the way we do things in the operating room (OR). For example, when a hospital adopts a high-reliable technology, like bar-code scanning of surgical sponges, it engineers the problem out of the system, making the problem of a retained sponge nearly impossible to occur. In fact, I am not aware of a single case of a retained sponge in any of the hundreds of US hospitals that use sponge-counting technology when the technology was used properly. That’s re-designing the delivery of care.”
Makary explained that better technology allows healthcare givers to focus more on the patient while also improving on efficacy and safety. “In the past, we’d beat on ourselves as surgeons and those around us to remember better, work harder, and always be mindful of potential hazards. With new technology, we can focus more on the patient while having a better safety net for errors. We should teach every healthcare provider about their personal responsibility in taking care of patients, instilling accountability for our actions. At the same time, we should recognize we are humans and we will always be humans. We make mistakes and should not pretend that we can’t. The ultimate questions is, ‘Can we design smarter hospital systems to minimize the consequences of human errors when they occur?’”
Solutions for surgery-related Never Events
Stryker offers a solution that employs bar coding to prevent retention of surgical sponges. Jason Davies, Senior Brand Manager, Stryker, talked about the serious consequences of a surgical sponge left inside a patient and how Stryker’s SurgiCount Safety-Sponge system achieves spectacular results in reducing the risk, potentially saving lives. “A retained surgical sponge—i.e., a sponge left inside a patient, often due to miscounting—is one of the most common Never Events. In the United States, it occurs about 11 times per day, and one in 20 cases causes death.
“Stryker’s SurgiCount Safety-Sponge System uses bar-coded surgical sponges, scanners, and software to confirm digitally the manual counts of surgical sponges by nurses and other operating-room staff, thus preventing sponges being left behind in patients,” stated Davies. “Hospitals have performed over 11 million procedures, using more than 200 million SurgiCount sponges, in the past five years without a single retained—surgical-sponge Never Event.”
Davies pointed out how use of technologies like Strykers’ can save hospitals money while improving patient safety. “Financial costs associated with Never Events come primarily from corrective surgeries and lawsuits in which patients seek financial reparations for harm done to them. Legal costs affect hospital budgets and constrain resources, because Centers for Medicare and Medicaid Services (CMS) and private insurers often refuse to reimburse for the costs of these errors. Compared with the estimated $600,000 in malpractice risk associated with a retained surgical item, the $8 to $10 cost per procedure to implement SurgiCount represents a significant cost savings.3 Medical malpractice impact per case of a retained surgical item in the United States adds $94.50 to the cost of a relevant surgery (roughly 9 times the cost of a sponge-counting technology).3
Davies cited a non-sponsored Mayo Clinic study on adjunct sponge-management technology that evaluated the SurgiCount system in 128 operating/procedure rooms across the Rochester campus beginning in February 2009.4 “Before implementation of SurgiCount, a retained sponge occurred on average every 64 days,” said Davies. “Between February 2009 and July 2010, 87,404 procedures were performed, and 1,862,373 bar-coded sponges were used without a retained surgical sponge being left behind. SurgiCount caused no workflow disruption or increases in case duration. Staff satisfaction was acceptable, with a high degree of trust in the system.”
Surgical checklists save lives
Another surgery-related Never Event in the top ten is wrong-site/wrong-procedure/wrong-patient events. Unquestionably, communication helps to reduce defects in the process, which reduces risk of wrong-site/wrong-procedure/wrong-patient events.
Makary and his research team developed and published the first surgery checklist to be used prior to a surgical procedure, along with a debriefing checklist to be used after the operation. It may sound like a simple solution, but they are very effective tools in preventing missteps or overlooking important steps in protocol. In fact, these checklists proved so effective in Johns Hopkins’ experience that, when results were presented to the World Health Organization (WHO), “they chose to adopt both in their version,” said Makary.
LiveData, Inc., developed LiveData Active Time Out (ATO) to help prevent adverse occurrences. Jeffrey Robbins, President and CEO, described the ATO as an electronic surgical-safety checklist developed with the intent of improving team communication by integrating checklists into surgical workflow.
“The WHO Surgical Safety Checklist and The Joint Commission Universal Protocol are accepted as standard tools to improve surgical safety,” said Robbins, “yet, checklists are not used for every surgical case. ATO ensures consistent and measurable use of the checklist and leads to improved patient safety and clinical quality.
“ATO presents the checklist before each of three critical surgery steps: anesthesia induction, incision, and patient leaving the OR,” explained Robbins. “LiveData ATO is displayed on monitors in the OR in view of all members of the surgical team. A team member—surgeon, circulating nurse, or other clinician—uses a wireless ‘clicker’ to step through the checklist and record responses.”
LiveData ATO is a component of LiveData PeriOp Manager, a solution that synchronizes the patient journey from clinic visit onto the surgical schedule and throughout the day of surgery. “Each step of the workflow is automated and tracked in real time to improve workflow efficiency and deliver detailed analytics,” noted Robbins.
“The Joint Commission projected 50 wrong-site, wrong-procedure, or wrong-patient incidents occur each week in the US,”5 Robbins added. “The cost of implementing ATO can be justified by eliminating financial losses from nonreimbursements and malpractice suits. A 2013 research study identified 9,744 malpractice settlements for surgical Never Events between 1990 and 2010, with payments totaling $1.3 billion.”6
Robbins referred to the Veterans’ Affairs (VA) Miami Healthcare System’s experience with LiveData ATO. “In 2014, VA Miami Healthcare System won Patient Safety Project of the Year in Health Data Management’s Analytics All Stars program. VA Miami verified that one month after implementing ATO, surgical-safety—checklist compliance increased dramatically with real-time data confirming that checklists were actively completed.”7
Preventing medication errors
Medication errors and healthcare-acquired infections (HAIs) are also top-ranking Never Events. Steve Riddle, PharmD, BCPS, FASHP, Director of Clinical Development, Wolters Kluwer, Pharmacy OneSource Solutions, explained how their company’s solutions help to reduce risk of both Never Events. “Pharmacy OneSource solutions address two categories of Never Events: HAIs.
“The Sentri7 clinical surveillance solution provides continuous, real-time analysis and aggregation of patient data, allowing clinicians to pinpoint patients at risk,” explained Riddle. “The system gathers critical information from electronic medical records (EMRs) and other disparate laboratory and clinical systems, and leverages rules-based algorithms to flag potential infection and antimicrobial issues. Alerts are then immediately delivered to clinicians along with evidence-based clinical-decision support to guide impactful clinical response.”
Riddle highlighted the experience of a multi-hospital network, with a presence in more than 20 states, that achieved impressive results within 18 months after deploying Sentri7: 95 percent increase in patient-care activities; 18 percent decrease in catheter-associated urinary tract infection; 7 percent decrease in central-line associated bloodstream infection; and, $16 million in annual savings.
Compounding, as a Never Event, has received considerable negative attention in recent history. Riddle explained that their solution helps healthcare organizations meet the strict requirements of “United States Pharmacopeia (USP)” chapter 797 and the recently published USP chapter 800. “Sterile compounding is a high-risk function, and contaminated solutions can cause significant patient harm. Simplifi 797 is a comprehensive quality-management system that addresses the complexities of sterile compounding processes used in generating certain medication treatments, most often for intravenous (IV) administration. By facilitating ongoing compliance with training, procedures, and documentation, the tool is essential to elevating patient safety and mitigating risk.”
Riddle added, “Recent high-profile sterile compounding disasters across the U.S., and the resulting increase in regulatory scrutiny, prioritizes the need for quality management systems like Simplifi 797. Along with promoting compliance with industry best practices, the solution also provides 33 CE credits of sterile-compounding training that ensure staff competency and maintenance of professional licensing.”
Concerning the risks accompanying medication errors, David Swenson, RPh, Vice President of Medical Affairs, BD, related, “An estimated 56 percent of medication errors are IV-related, and 61 percent of these errors are life-threatening.8 For optimal infusion safety, and to reduce the likelihood of an IV medication error reaching the patient, it’s imperative that hospitals take a systems-based approach to IV therapy by looking at the entire infusion process, from compounding in the pharmacy to administration at the bedside, ensuring both technologies and workflows are optimized and integrated with the EMR.
“Traditional infusion practices present ample opportunities for error,” stated Swenson. “National data tell us that 7 percent of high-risk IVs are compounded in error.9 In addition, 68 percent of medication errors occur during the administration phase, and 20 percent of those are due to manual infusion-pump programming.”10
Swenson said that the BD Cato system uses gravimetric analysis, bar-code verification, and hard stops to detect potential medication errors in real-time during compounding. He referred to a one-year independent study at MD Anderson (University of Texas MD Cancer Center), which revealed that, by using BD Cato, there were 7.1 percent errors detected, representing a 74-fold increase in errors caught by the system.9
Swenson explained how BD’s Alaris EMR Interoperability reduces chances of errors and supports compliance with The Joint Commission and CMS requirements. “With interoperability, infusion-pump parameters are pre-populated from the EMR, reducing manual key presses, and infusion-status data is sent from the pump back to the EMR within seconds, providing a single reliable record of the entire IV therapy—every titration, start, and stop.”
The costs in human suffering and deaths, as well as the financial costs to the hospital, due to medication errors is staggering, noted Swenson. “Adverse drug events result in more than 770,000 injuries and deaths each year and cost up to $5.6 million per hospital, depending on size.11 There is also the risk of lost revenue due to inaccurate infusion documentation.” Swenson cited the example of SCL Health-St. Vincent Healthcare, which saw reduced lost infusion revenues by 16.8 percent soon after interoperability implementation. “Biltoft noted that ‘perfect documentation’ can help the health system capture the $4 million in infusion charges that were being missed annually, before implementation of interoperability,” said Swenson.12
Communication is key
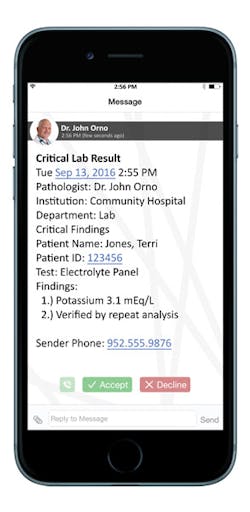
Unquestionably, lack of communication and a delay in appropriate treatment can contribute to Never Events. Andrew Mellin, MD, Chief Medical Officer, Spok, related how Spok Care Connect integrates with existing hospital workflows and systems to enable clinicians to receive the information they need quickly and securely on a range of mobile devices, including smartphones, pagers, and Wi-Fi phones. “This healthcare communications platform speeds communications in a variety of ways — such as automating the delivery of critical test results from cardiology, laboratory, and radiology — to the ordering physician’s device and updating the patient’s EHR with an audit trail. This rapid information sharing works to prevent lost results or delays in treatment because results take too long in transit between departments, situations that constitute a care-management Never Event.
“Many organizations currently use manual procedures to communicate and log critical test results process steps,” continued Mellin. “There can be a lot of back and forth with voice mails between the physician or technician who interpreted the test and the one who ordered it. In rare cases, critical results are not communicated to the right person or with the right urgency, leading to patient harm. With the chance of patient death or serious injury resulting from failure to follow up or communicate laboratory, cardiology, or radiology test results, it’s important to both patient care and the hospital’s reputation to put steps in place to prevent these situations.”
Mellin explained that Spok Care Connect is effective not only in helping health systems prevent Never Events related to lost or delayed test results, “but also for improving everyday communications and workflows that strengthen patient satisfaction and staff efficiency. All hospitals are looking to avoid mistakes, lawsuits, and expensive settlements, which can cause a loss of trust in the community. Spok supports more than 1,900 hospitals—both large and small—in their quest to deliver the highest standards of care with communication technology designed to meet today’s challenges. The enterprise-wide capabilities of Spok Care Connect make it a cost-effective choice for health systems looking to bolster many aspects of communications and promote positive patient experiences.”
Looking ahead
Where do we go from here? Makary and his team continue to focus on making health care safer and more efficient, including finding ways to save money within the system, money that may be used to improve quality of patient care. “Never Events rose to the forefront of patient-safety discussions in health care because there is uniform consensus they should never occur regardless of the situation,” stated Makary. “We should now ask are medical centers adopting a process or technology to prevent them from occurring, and are we seeing an improvement?
“The field of quality of safety has learned a lot from the early Never Event metrics of performance,” continued Makary. “The future will usher in many more. My research team is now focused on developing additional meaningful quality metrics for health care; specifically, ones that are patient-centered, endorsed by physicians in the specialty being measured, and capture wasted dollars in the system. Our new home-grown ‘Appropriateness Measures’ are being used in health systems to ask, ‘How often is surgery performed appropriately at your medical center, and where is the waste?’ We currently have 50 metrics of waste that can be derived from billing or clinical data. Already, hospitals are saving money from the effort, enabling them to spend more money on important patient-safety and quality initiatives.”
References
1. U.S. Department of Health and Human Services. Agency for Healthcare Research and Quality. Patient Safety Network. Never Events. https://psnet.ahrq.gov/primers/primer/3/never-events. Last updated July 2016. Last accessed April 28, 2017.
2. Snowdon A, Alessi C. World Health Innovation Network Visibility Thought Paper. Visibility: the new value proposition for health systems. https://issuu.com/worldhealthinnovationnetwork/docs/full_paper_-_win_visibility_thought/1?e=25657717/39177387). Pages 13-14; 25. Last accessed April 29, 2017.
3. Sloane T. The high cost of inaction: retained surgical sponges are draining hospital finances and harming reputations. Becker’s Infection Control & Clinical Quality. August 12, 2013. http://www.beckershospitalreview.com/quality/the-high-cost-of-inaction-retained-surgical-sponges-are-draining-hospital-finances-and-harming-reputations.html. Last accessed April 20, 2017.
4. Cima RR, Kollengode A, Clark J, et al. Using a data-matrix—coded sponge counting system across a surgical practice: impact after 18 months. Jt Comm J Qual Patient Saf. 2011(Feb);37(2):51-58.
5. Chassin MR, Loeb JM, The Joint Commission. High-reliability health care: getting there from here. http://www.jointcommission.org/assets/1/6/Chassin_and_Loeb_0913_final.pdf. Last accessed May 1, 2017.
6. Mehtsun, WT, Ibrahim AM, Diener-West M, et al. Surgical never events in the United States. Surgery. 2013(Apr);153(4):465-472.
7. HealthData Management. Project of the year, patient safety: VA Miami Healthcare System. https://www.healthdatamanagement.com/news/hdm-names-2014-analytics-all-stars. Last accessed April 25, 2017.
8. Prusch A, Suess T, Paoletti R, et al. Integrating technology to improve medication administration. Am J Health Syst Pharm. 2011;(May);68(9):835-842. http://www.ajhp.org/content/68/9/835.short. Last accessed May 2, 2017.
9. Reece KM, Lozano MA, Roux R, et al. Implementation and evaluation of a gravimetric iv. workflow software system in an oncology ambulatory care pharmacy. Am J Health Syst Pharm. 2016;73:165-173.
10. California Hospital Patient Safety Organization. ECRI Institute PSO deep dive analyzes medication events. Patient Safety News. 2012(Oct);4(9). http://www.chpso.org/sites/main/files/file-attachments/201210.pdf. Last accessed May 3, 2017.
11. Agency for Healthcare Research and Quality. Reducing and preventing adverse drug events to decrease hospital costs. Publication # 01-0020. March 2001. https://archive.ahrq.gov/research/findings/factsheets/errors-safety/aderia/ade.html. Last accessed May 2, 2017.
12. Wild D. Smart pumps and EHRs can play nice. Pharmacy Practice News. 2015(Sep);42(9).
About the Author

Susan Cantrell
Susan Cantrell is Infection Prevention Editor for Healthcare Purchasing News.