Doctors, nurses and healthcare teams make a pledge to “do no harm” to patients. Whether practicing emergency, surgical or routine care, the goals remain the same – to perform the most effective and safe treatment and improve health, comfort and satisfaction for every patient.
Catheter placement and infusion therapy typically require the use of invasive devices. These, of course, pose health risks in care, including potentially dangerous or deadly infections. The ongoing COVID-19 pandemic also creates additional hurdles in acquiring vital supplies and equipment needed for patients.
So, what kinds of situations may arise when delivering this care? And what are the most useful products and best practices recommended to achieve safe and successful outcomes?
Preventing complications
Education and compliance
“COVID-19 has increased the number of intravenous devices used during this pandemic surge,” Moureau indicated. “The increasing need for intravenous device insertions and crisis management has negatively affected outcomes and the ability to purchase better products or apply performance improvement initiatives. Overall, we have seen an increase in device-related complications as a result of COVID-19.”
Other circumstances, Moreau observes, are patient choices around treatment and the risk of COVID-19 infection.
“Patients have all been scared, especially those with chronic or genetic disorders, while receiving treatment in or out of the hospital,” she explained. “Two patients of mine receive long-term intravenous treatments and are at higher risk for COVID-19. One of these patients is very careful and compliant with distancing and day-to-day activities resulting in more stability, while the other is noncompliant. The noncompliant patient has experienced multiple hospitalizations and is exposed to greater risk to his health status. Using all the best products to ensure safety and positive outcomes still requires constant education of the patient and caregivers with a goal of optimal health.”
Staff should receive adequate education on tools and processes in order to benefit care and patients, Moreau continues.
“We know from the published research that using reflux-limiting needleless connectors reduces catheter failure and other complications,” she noted. “Education focused on using effective flushing techniques and correct clamping sequences for needleless connectors helps to minimize thrombotic occlusions, but what we have found is that education does not reach everyone and needs to be reinforced over and over. As technology increases in healthcare, it is necessary to provide evidence-based education to clinicians on how to safely and efficiently perform management and care of devices used for treatment.”
Specialty teams and technology
At Hartford Hospital, part of the Hartford Healthcare system in Hartford, CT, they concentrate on techniques that help lower the risk of complications, maintain devices, and manage costs in care, expresses Lee Steere, RN, CRNI, VA-BC, Unit Leader IV Therapy Services.
“Our goal is to increase first-time insertion success and reduce preventable complications in order to make vascular access devices last longer,” Steere said. “Part of this involves centralizing IV therapy services – including catheter selection, insertion and management – within a vascular access specialty team (VAST) of experts. As a result, we have decreased our catheter consumption, which can help avoid any sourcing or supply issues that may arise. In addition, our experience has shown this approach can increase patient satisfaction, improve clinical outcomes and reduce costs associated with infusion therapy.”
One problem that can occur and be prevented is a catheter occlusion, addresses Steere.
Both technology and practices have improved the hospital’s care and bottom line, continues Steere.
“A study of this model found higher IV success rates, longer dwell times and fewer complications, which translated to an 80 percent reduction in catheter consumption and a projected annual savings of $2.9 million,” he indicated.1 “For CVADs, the anti-reflux device helped reduce occlusions by 69 percent, while also lowering needleless connector consumption by 51 percent. Overall, we estimate an annual savings of more than $250,000 by reducing occlusions and CLABSIs, as well as the use of alteplase, heparin and other supplies.” 2
Device maintenance and disinfection
Another focus for hospitals and healthcare facilities is keeping medical supplies and equipment in working order, clean and sterilized for use on patients.
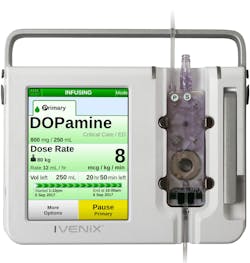
“Even before COVID, today’s infusion pump market was already strained due to FDA recalls and warnings for hardware and software errors, cybersecurity gaps, and issues relating to more stringent cleaning practices,” emphasized Susan , MHA, BSN, RN, Chief Nursing Officer, Ivenix, Inc., North Andover, MA. “The pandemic also has emphasized an important element of medical device products: the materials in which the devices are made of matters. To prevent infection, devices that withstand frequent, harsh chemicals used to disinfect between patients are key. Devices with ingress protection and few crevices to trap contaminants are equally important to prevent transmission of infectious pathogens.”
Michele Padovan, Clinical Nurse Specialist, Angelini Pharma, Inc., Rockville, MD, addresses the importance of catheter disinfection with dialysis treatment.
“Tunneled, central venous catheters are meant for long-term use in the hemodialysis patient (months to years), making them high-risk implantable items in an immune-suppressed patient,” Padovan stressed. “It is critical that the catheter is accessed aseptically for dialysis and that the exit site is kept clean and dry. For some dialysis patients, this CVC will remain their sole access for treatment if they have exhausted all peripheral means for phlebotomy. Alcavis 50 is a high-level disinfectant with a broad and rapid kill and ExSept Plus is an isotonic catheter exit site cleanser; both products are safe and effective with a long history of use on catheters. The Alcavis Bleach Wipes are chlorine-based surface disinfectants in three dilutions for a variety of hard surfaces, including infusion pumps and poles.”
Further, the company provides cleaning and sanitizing products for other items in healthcare environments, expresses Padovan.
“Over the past eight months, Angelini Pharma has seen a remarkable increased interest from customers requesting products that facilitate antisepsis and disinfection in their facilities,” she continued. “This includes products for catheters, skin, hands and surfaces. A dialysis facility relayed to us that the addition of the Alcavis Bleach Wipes to disinfect frequently touched surfaces, such as countertops, waiting room furniture, and doorknobs, has given their patients a sense of comfort while they are in the facility. The nurse stated that her patients are less concerned coming in for their treatments, seeing that staff have implemented this procedure with regularity.”
Protecting patients and staff
Rapid care
Controlling the transmission of COVID-19 among patients, staff and visitors remains top of mind in medical settings. The crisis, however, has taken a major toll on necessary medical and personal protective equipment (PPE) items, emphasizes Karoline Draper, RN, MSN, VA-BC, Smiths Medical, Minneapolis, MN.
“Our healthcare customers are currently struggling under the weight of extremely sick and contagious patients,” Draper shared. “They are overwhelmed and under financial strain, making it more difficult to allocate resources to much needed supplies.”
The company’s POWERWAND family of products offers up to 90 percent completion of therapy for medication delivery, diagnostics and blood sampling, resulting in more efficient care 3, notes Draper.
“We have seen a lack of PPE for healthcare workers during COVID-19,” Draper said. “To keep nurses safe and prevent spread, clinicians are leaning on products like our POWERWAND midlines and extended dwell catheters to decrease utilization of PPE, by helping achieve one-stick hospitalization, and less time spent in COVID-19 rooms. 3-4 The POWERWAND midline catheters can be placed in patients upon admission to the hospital and/or COVID-19-specific units. This practice has been implemented in facilities with the intent to decrease delays of care, improve patient outcomes,4 protect staff from unnecessary exposure with restarts1 and reduce PPE usage.”
Managing supplies and care
Increased inventory needs
As the COVID-19 global public health emergency carries on, so does the pressure on healthcare supply chain and critical care operations, observes Matthew Hutchings, VP Global Marketing and Innovation, Infusion Systems, ICU Medical, San Clemente, CA.
“Hospitals around the world have not only experienced unprecedented surges of critically ill COVID-19 patients, but this uncertainty and variability in patient volumes have also put significant stress on the healthcare supply network,” Hutchings addressed. “At the onset of the pandemic, a rapid increase in patient volumes, coupled with the stockpiling of essential infusion consumables, created back orders and supply shortages — from PPE to core infusion sets and infusion pumps. In contrast, the volumes of elective surgeries are still far below pre-pandemic levels, placing additional financial burdens on hospitals and healthcare facilities.”
The change in seasons and viruses, Hutchings indicates, will heighten tension on healthcare systems, supply availability, and capacity for treatment.
“The fall and winter months are traditionally very busy for healthcare suppliers, as hospitals and healthcare facilities stock up on essential supplies for treating seasonal flu patients,” he emphasized. “As COVID-19 continues to draw much of the supply from the healthcare supply chain network, already-stretched manufacturers may face additional challenges. It’s clear that healthcare suppliers will continue to fare differently as those that built additional supply early on may have an advantage in maintaining a consistent, reliable supply of essential infusion products to help healthcare providers weather this evolving storm. Also, the increased pressure to stockpile supplies has left many with limited space. As a result, many now rely on manufacturers and vendors, like ICU Medical, to be more of a warehouse, supplying them timely as massive spikes in COVID-19 patients increase demand.”
Katie Szyman, Corporate Vice President, Critical Care, Edwards Lifesciences, Irvine, CA, suggests that medical manufacturers must shift production accordingly in order to meet needs during the continuing crisis.
For example, Szyman, added, “We saw that the COVID-19 pandemic caused hospitals to expand ICUs, which in turn created a high demand for critical care equipment, including products such as our HemoSphere advanced hemodynamic monitor, Swan Ganz catheter, pressure transducers, etc. In a normal year, according to the CDC, the flu season alone can impact up to 11 percent of the U.S. population. As hospitals work to treat patients with these two diseases, which both impact the respiratory system, we may see an even higher need for medical technologies. This could lead to hospitals being once again overwhelmed and having to manage ICU space to care for critically ill patients.”
AI and data
Technology, like artificial intelligence (AI), may become a greater resource in care, observes Szyman.
“AI has been a buzzword for a while now, but I think we’re really starting to see some technologies come to market that are using AI wisely in a way that rapidly analyzes a lot of data to quickly give clinicians valuable information,” she explained. “A big focus for us is advancing our hemodynamic monitoring platforms with predictive software, and we are also evolving these systems to support remote monitoring, giving clinicians even more access to patient data beyond the bedside. The move to less-invasive and noninvasive devices is another area that isn’t new, but the need is heightened by COVID-19.”
Adapting processes, settings
Versatile care
As intensive care has risen during the COVID-19 pandemic, many hospitals have reallocated supplies and adjusted protocols and practices, addresses Niemeier.
“One such practice change was to move infusion pumps away from the bedside and into the hallway, enabling clinicians to limit contact frequency and conserve critical PPE while treating COVID patients,” she indicated. “This also allows clinicians to easily manage multiple IV lines and infusions, especially those that contain life-sustaining medications for which even a brief pause in delivery could be tragic. To increase the length of IV tubing, multiple extra-long extension sets are connected together to reach the patient, which has resulted in skyrocketing demand for extension sets for this modified workflow. In addition, the increased demand for additional IV accessories – fluids and dedicated IV tubing, for example – has also increased.”
She points to several examples of what has been valuable for safe and effective care in this era, including:
• Accurate infusion drug delivery under changing clinical conditions – regardless of extension sets, position to the pump-to-patient, and viscosity of the medication;
• Remote clinical viewers that allow clinicians to see their patient’s status, if alarm conditions exist, and help ensure life-sustaining infusions are not interrupted due to a low IV bag;
• The latest drug library updates – automatically delivered within minutes and without disruption to care; and
• The availability of clinical resources and educational materials on the pump, reinforcing COVID safety guidelines and drug regimens, reducing confusion and providing safer care.
With regard to patient procedures, various supplies, equipment and modes may be used to support safety and infection prevention, explains Harrison Richards, Director of Marketing, IV Consumables, ICU Medical, San Clemente, CA.
“One option is using gravity IV sets with integrated manual flow controller devices,” Richards expressed. “These devices allow healthcare providers to administer medications safely when access to IV pumps may be limited. While IV therapy is essential to COVID-19 patient care, accessing these patients’ bloodstreams may increase infection risk. Consequently, minimizing entry points for bacteria with needlefree connectors, such as our Clave needlefree IV connector technology, can be an essential to helping reduce the risk of bloodstream infections. Additionally, the FDA recently authorized monoclonal antibody treatments for emergency use to treat mild-to-moderate COVID-19 in adult and pediatric patients. The recommendation is to administer these treatments through polyvinyl chloride (PVC) infusion sets containing 0.20/0.22 micron in-line polyethersulfone (PES) filters.” 5-6
Virtual training
Going virtual has become an essential part of healthcare and manufacturing training and business during the crisis.
“We are adapting product training and education to a virtual environment, which has become crucial for our customers in today’s healthcare setting,” Draper shared.
Online platforms can help improve time and efficiency in service, addresses Niemeier.
“From a vendor’s perspective, we are changing the way we market and deploy our products,” she explained. “In one recent experience, we virtualized our whole model of implementation. Our project kick-offs, design and build sessions for the infusion management system, the drug library and configurations, and testing were all done via a virtual conference platform. We utilized computer-based training to replace the majority of what is done in a classroom and were able to reduce the amount of on-site time to less than 10 percent.”
Further, virtual platforms have strengthened customer partnerships and connections, stresses Syzman.
“With the recent pandemic, our customers have appreciated our hands-on approach to outfitting ICUs with our products and providing comprehensive training, even if virtual,” she said. “In addition, we have seen clinicians from other areas, such as OB/GYN specialists, needing to help out in the ICU. As a result, we’ve seen a surge in usage of remote training online for our products as well as increased links to social media for “refresher courses” of how to place catheters to monitoring patients in the ICU.”
References
1. Steere, L. Ficara, C. Davis, M. Moureau, N. Reaching One Peripheral IV Per Patient Visit with Lean Multi-Modal Strategy: The PIV5Rights Bundle. JAVA. 2019;24(3):31-43. Link to Study
2. Steere, L. Lean Six Sigma for Intravenous Therapy Optimization: A Hospital Use of Lean Thinking to Improve Occlusion Management. JAVA. March 2018. Vol 23 No 1. Pg. 42-50. Link to Study
3. AV Caparas J. Staff Education/Training Aids Implementation of Advanced Midline Catheter. Poster presented at 2013 Infusion Nurses Society Annual Convention and Industrial Exhibition.
4. Bird D. The Power of Choice: Midline Catheter Improves Patient Safety and Comfort While Increasing Vascular Access Revenue and Productivity. Poster presented at 2012 Association for Vascular Access Annual Scientific Meeting.
5. Diamond, Frank. “Study: CLABSI, CAUTI Rates Higher for COVID Patients.” Infection Control Today, 21 Oct. 2020, www.infectioncontroltoday.com/view/study-clabsi-cauti-rates-higher-for-covid-patients.
6. McMullen, Kathleen M., et al. “Impact of SARS-CoV-2 on Hospital Acquired Infection Rates in the United States: Predictions and Early Results.” American Journal of Infection Control, vol. 48, no. 11, 1 Nov. 2020, pp. 1409–1411, www.ncbi.nlm.nih.gov/pmc/articles/PMC7329659/, 10.1016/j.ajic.2020.06.209.
About the Author

Ebony Smith
Ebony Smith was previously Managing Editor for Healthcare Purchasing News.